Heel Pain: Understanding the Causes and Effective Solutions for Relief
Heel pain is a common complaint that can significantly impact daily life. Whether you’re an athlete, a busy professional, or someone who enjoys leisurely walks, experiencing heel pain can be debilitating. The question “why does my heel pain?” is one that many people ask, and the answer can vary widely depending on the underlying cause. In this article, we will delve into the various factors that contribute to heel pain, explore scientific explanations, and provide practical solutions for relief.
:max_bytes(150000):strip_icc()/heelpainfinal-01-5c86a48246e0fb00014319ff.png)
Common Causes of Heel Pain
One of the most common causes of heel pain is plantar fasciitis. According to the American Academy of Orthopaedic Surgeons, plantar fasciitis is the inflammation of the plantar fascia, a thick band of tissue that runs across the bottom of your foot and connects your heel bone to your toes. This condition often results from overuse, such as excessive running or standing on hard surfaces for long periods. The pain is typically worse in the morning when you take your first steps, as the plantar fascia tightens overnight.
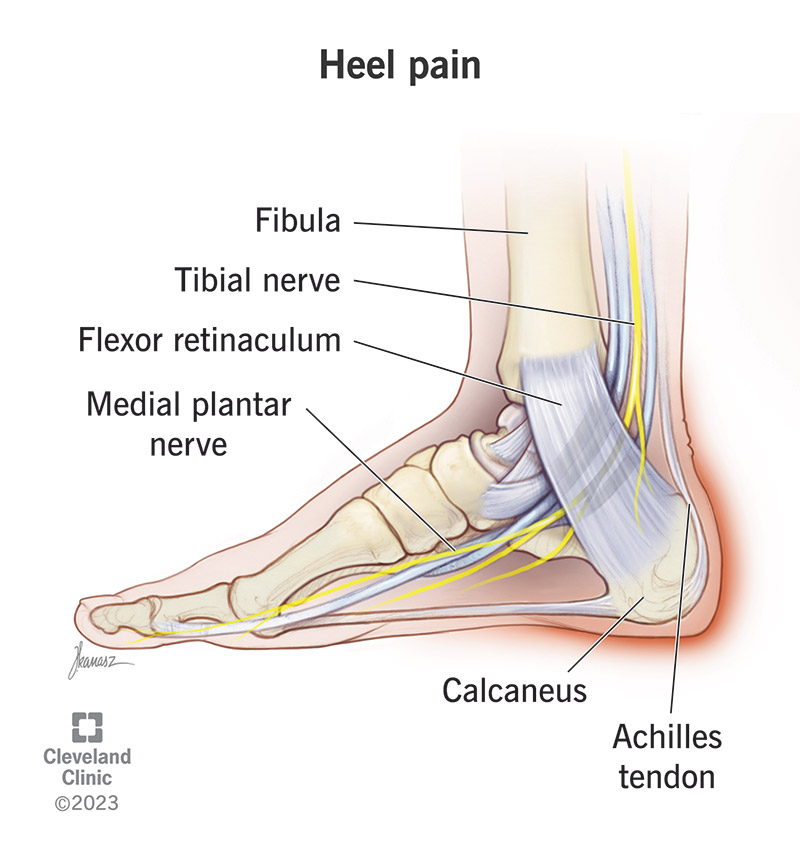
Another frequent cause of heel pain is Achilles tendonitis, which involves inflammation of the Achilles tendon, the band of tissue that connects your calf muscles to your heel bone. This condition is often seen in runners and people who engage in activities that require sudden starts and stops. The pain is usually felt at the back of the heel and can be exacerbated by activities that strain the tendon.

Diagnosing Heel Pain
Diagnosing the cause of heel pain often requires a comprehensive evaluation by a healthcare professional. This may include a physical examination, medical history review, and possibly imaging studies such as X-rays or MRIs. Dr. James Ioli, a podiatrist at Harvard Medical School, emphasizes the importance of a thorough assessment: “Understanding the specific cause of heel pain is crucial for effective treatment. Each condition has its own set of symptoms and requires a tailored approach.”
For instance, a physical examination can help identify tenderness, swelling, or redness around the heel area. Medical history can reveal factors such as recent changes in activity level, footwear, or any previous injuries. Imaging studies can provide detailed views of the bones, tendons, and soft tissues, helping to rule out more serious conditions such as stress fractures or bone spurs.

Effective Solutions for Relief
Once the cause of heel pain is identified, a variety of treatment options are available. Conservative treatments are often the first line of defense and can include rest, ice, compression, and elevation (RICE method), as well as over-the-counter pain relievers like ibuprofen or naproxen. Stretching exercises can also be beneficial, particularly for conditions like plantar fasciitis and Achilles tendonitis. Dr. Jordan Metzl, a sports medicine physician, recommends specific stretches: “Stretching the calf muscles and the plantar fascia can help reduce tension and alleviate pain. Incorporating these stretches into your daily routine can make a significant difference.”
In some cases, custom orthotics or supportive footwear may be recommended to provide additional support and cushioning. Orthotics can help redistribute pressure across the foot, reducing strain on the heel. Additionally, physical therapy can be an effective treatment option, focusing on strengthening the muscles and improving flexibility.

When to Seek Professional Help
While many cases of heel pain can be managed with self-care measures, there are situations where professional help is necessary. If your heel pain persists for more than a few weeks despite conservative treatment, it may be time to consult a healthcare professional. Persistent pain, swelling, or redness, as well as difficulty bearing weight on the affected foot, are signs that you should seek medical attention.
In some cases, more invasive treatments such as corticosteroid injections or surgery may be considered. However, these options are typically reserved for severe cases that do not respond to conservative treatments. Dr. David Geier, an orthopedic surgeon, advises: “It’s important to explore all conservative treatment options before considering more invasive procedures. Many cases of heel pain can be successfully managed without surgery.”
Preventing Heel Pain
Preventing heel pain involves a combination of good footwear, proper stretching, and moderation in physical activity. Choosing shoes with good arch support and cushioning can help reduce the risk of developing heel pain. Regular stretching exercises, particularly for the calf muscles and plantar fascia, can also play a crucial role in prevention.
Maintaining a healthy weight and avoiding sudden increases in activity level can further reduce the risk of heel pain. Dr. Nicholas DiNubile, an orthopedic surgeon, emphasizes the importance of gradual progression: “Gradually increasing your activity level allows your body to adapt and reduces the risk of overuse injuries like plantar fasciitis and Achilles tendonitis.”
:max_bytes(150000):strip_icc()/heelpainfinal-01-5c86a48246e0fb00014319ff.png)
In conclusion, understanding the causes of heel pain and implementing effective solutions can lead to significant relief and improved quality of life. Whether you’re dealing with plantar fasciitis, Achilles tendonitis, or another condition, a comprehensive approach that includes proper diagnosis, conservative treatment, and preventive measures can help you overcome heel pain and get back to your daily activities.